With many people suffering with ongoing symptoms following a COVID-19 infection, there is understandably a lot of interest in the role that nutrition may play in recovering from or dealing with ongoing symptoms. This article will explore nutrition considerations related to Long-COVID*.
*Note: This article is not covering the nutritional management of an acute COVID-19 infection. Please follow the individual advice you have received from your doctor and healthcare team if you are suffering with Long-COVID.
What is Long-COVID?
Long-COVID or Post-COVID Syndrome is defined as “signs and symptoms that develop during or following an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis” (1).
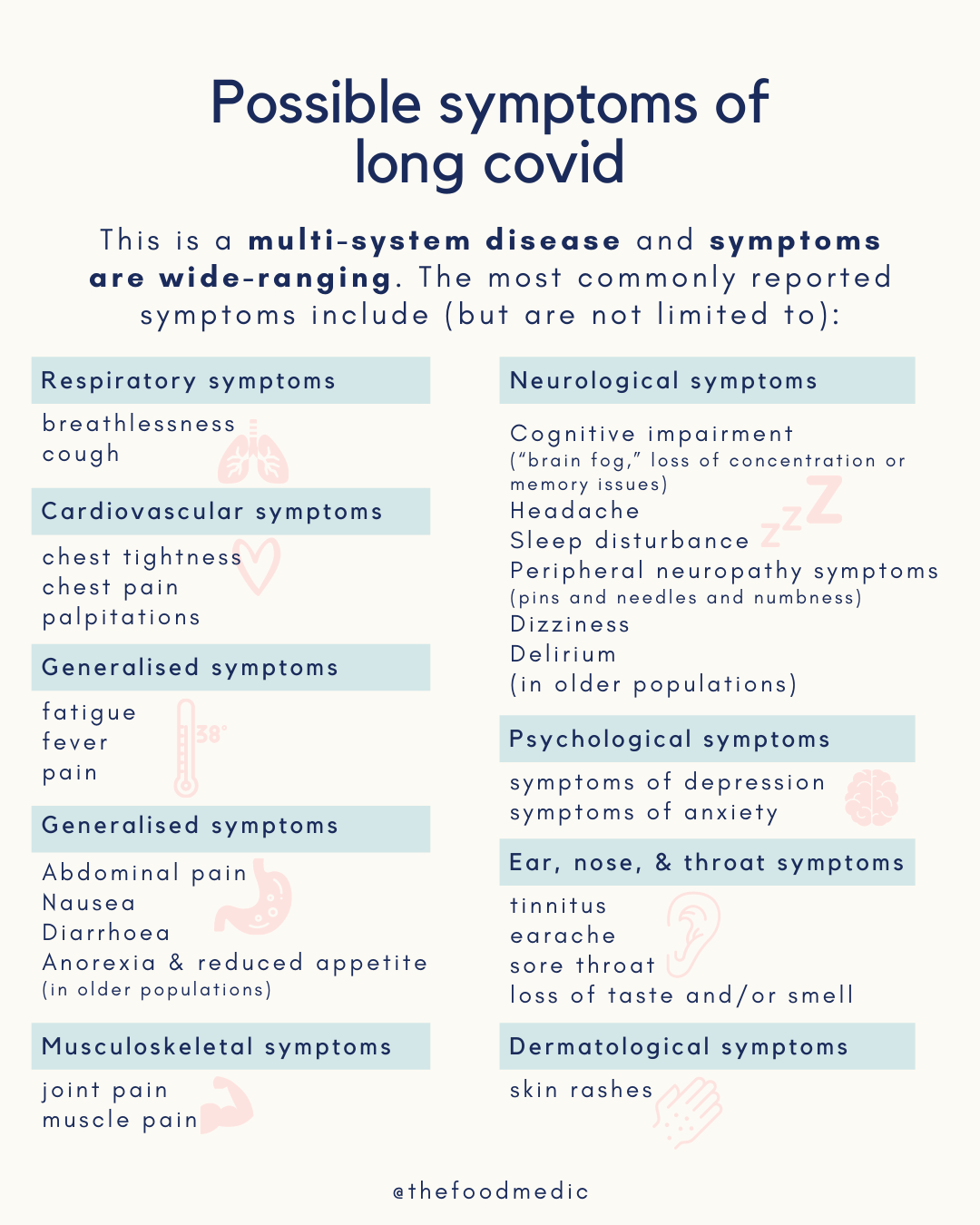
Image reference: Managing the long term effects of covid-19: summary of NICE, SIGN, and RCGP rapid guideline, BMJ (2021)
We are still learning a lot about Long-Covid but what we know so far is that the chances of having long-term symptoms does not seem to be linked to how ill you are when you first get COVID-19. People who had mild symptoms, can still experience long-term health problems as a result. Recovery time from COVID-19 is different for everyone and is rarely linear with symptoms often fluctuating. If you’re worried about symptoms 4 weeks or more after having COVID-19 contact your GP for an initial telephone consultation. They can offer you the support you may need.
Long-COVID and Nutrition
Based on the current evidence, there is no specific diet that prevents or cures COVID-19 infection or Long-COVID.
It is important to highlight that many of the diets that some people are promoting as a cure for Long-COVID are restrictive and cut out a lot of foods, which comes with additional nutritional risks to consider.
One diet that has gained some attention related to Long-COVID is the low-histamine diet. It is thought that Mast Cell Activation Syndrome may play a role in Long-COVID, and mast cells release histamine; a chemical related to inflammation (2, 3). Histamine is also found in certain foods, hence the suggestion that a low histamine diet may be helpful in the management of Long-COVID.
Here are some examples of high-histamine foods:
- Cured and aged meat
- Oily fish and shellfish
- Fermented dairy including aged cheese, yogurt and kefir
- Eggs
- Deli chicken and turkey slices
- A number of fruit and vegetables, spices, nuts and fermented foods
But this is a theory and there is currently no direct evidence to support it. Furthermore, as the low-histamine diet is also very restrictive, so it isn’t suitable for everyone and should only ever be trialled for a limited amount of time with close support and supervision from a Registered Dietitian.
The Mediterranean-Style Diet:
Although there is currently no evidence related to the Mediterranean Diet and COVID-19 or Long-COVID, this is a balanced way of eating that is linked with numerous health benefits; including reduced inflammation (4). Therefore, this may be a sensible way of eating for many people with Long-COVID.
There is also a UK trial currently underway that is investigating the impact of phytochemicals (which the Mediterranean diet is high in) and probiotics to see whether this shortens the severity and duration of COVID-19 (5).
Here are some tips for following a Mediterranean-style diet:
- Aim for at least 5 portions of colourful fruit and vegetables a day; ideally aiming for more vegetables than fruit overall, but both fruit and vegetables are really good for you. Include 1-2 servings at each meal and swap your usual snacks for chopped up vegetables or a piece of fruit.
- Include 1-2 portions of oily fish per week in your diet, such as salmon, sardines, anchovies, trout, herring, pilchards, sprats and mackerel, which are rich in omega 3 and a good source of protein. If you’re not a fish eater, you can find omega 3 in walnuts, chia seeds, pumpkin seeds, flaxseed, soya products (like tofu, edamame beans and soya drinks/yogurts), rapeseed oil or omega-3 supplements.
- Try to reduce red and processed meat consumption by having 1-2 meat-free days per week. You could try to swap half (or all) of the mince meat in dishes (such as bolognese, chilli con carne, burgers, and cottage pie) for lentils, beans or quinoa.
- Add beans, lentils, and chickpeas to salads, soups, stews, and pasta dishes for additional fibre and protein.
- Eggs, shellfish and dairy are other nutritious options that are consumed in moderate amounts on the Mediterranean diet.
- Choose whole grains at most meals such as brown rice, wholemeal pasta, wholemeal bread, quinoa, buckwheat and porridge oats.
- Have a small handful of nuts per day, as these are a good source of healthy fats, fibre, protein, vitamins, minerals and antioxidants. All nuts provide slightly different nutrients so it’s a great idea to mix it up by eating mixed nuts or buying different types of nuts at each food shop. Adding mixed seeds on top of meals is another way to boost the nutritional content of a meal.
- Use olive oil as your main cooking oil and drizzle a little over salads you only need a small amount.
- Use herbs and spices to flavour meals rather than salt. Mixed spices and curry powder can contain added salt, whereas single herbs and spices usually don’t contain added salt.
- Consume smaller amounts of foods that are higher in saturated fat, sugar and salt such as biscuits, cakes, crisps, fried foods, and salted nuts. These don’t need to be entirely avoided, but eaten in smaller amounts and less often.
- Water is the main drink that is consumed on the Mediterranean diet, but tea and coffee also contain antioxidants and count towards your daily fluid intake.
- Red wine is the main type of alcohol that is consumed on the Mediterranean diet, and has been found to have anti-inflammatory properties — but this is only encouraged as an option if you already drink alcohol as there are health risks associated with consuming any amount of alcohol (6, 7). It is also advised to consume no more than 14 units of alcohol with at least 2 alcohol-free days per week (7).
It is important to take care of your overall wellbeing to support your immune system and health; and daily movement and socialising are actually part of the Mediterranean diet/lifestyle. Taking care of our immune health also includes prioritising stress management and sleep.
Vitamin D
There is some emerging evidence about the possible role of vitamin D in reducing the risk and severity of COVID-19 infection (8).
Although there is not enough evidence to establish a ‘cause and effect’ link between vitamin D and COVID-19 risk or outcomes, the National Institute for Clinical Excellence (NICE) recommend that those over the age of 4 should consider taking a daily supplement containing 10 micrograms of vitamin D to maintain bone and muscle health (8). This is recommended during October to March, or year round for those who have little to no sunshine exposure, including due to “spending most of [your] time indoors because of the COVID‑19 pandemic” (8).
Other Nutritional Considerations
For those who have spent time in hospital or been very unwell with COVID-19, issues with appetite or weight loss may have occurred. Eating enough food to build up strength and fuel the immune system is really important. Therefore individual support from a Registered Dietitian may be needed by those who are struggling with these issues.
Nutrition tips for a poor appetite:
- Eating small and often i.e. a. small meal or snack every 1-2 hours
- Avoid filling up on low-energy fluids like water or diet drinks, or lots of high fibre foods like having large portions of fruit and vegetables.
- Try nourishing drinks like milk, milkshakes, milky coffee, hot chocolate or smoothies.
- Fortifying meals and snacks by adding in extra: oil, milk, butter, cream, cheese, nut butter, ice-cream, jam, honey, sugar etc.
Ageusia and Anosmia
A loss of taste (ageusia) or smell (anosmia) is commonly reported post-COVID-19. In this case, experimentation with different flavours, types, textures and temperature of food may be helpful. Some of the above tips about eating with a poor appetite may also be useful if a loss of taste is impacting the enjoyment of food.
Smell training has been shown to help recovery in a number of studies, and the Royal College of ENT recommends this for everyone with anosmia that last more than two weeks (9). This involves repeated stimulation of the smell nerves. There are some free resources available to help you do this – check out the FifthSense or Abscent websites.
Summary
There is currently little to no evidence to support a particular way of eating for the management of Long-COVID. However, based on the overall available evidence related to nutrition, health and the immune system it seems sensible to consider a Mediterranean-style diet and vitamin D supplementation. Individual nutrition-related issues such as a poor appetite, weight loss or a suspected histamine intolerance should be treated with support from a Registered Dietitian.
Source: https://thefoodmedic.co.uk/2021/05/nutrition-and-long-covid/